Do you know that Diabetic retinopathy is the most common cause of vision loss for people with diabetes? It’s in fact, the leading cause of blindness for all adults in the U.S. Diabetic retinopathy is an eye condition that causes changes to the blood vessels in the retinal part of your eye. That’s the lining at the back of your eye that transforms light into images. The blood vessels can swell, leak fluid, or bleed, which often leads to changes in vision or blindness. It usually affects both eyes. When left to itself sans any treatment, diabetic retinopathy can blemish and damage your retina.
Symptoms of Diabetic Retinopathy
There are almost no signs you get to see until it becomes serious. When you do have symptoms, you might notice the following:
- Loss of central vision
- Inability to see colors
- Blurry vision
- Holes or black spots in your vision
- Small spots in your vision caused by bleeding
Causes
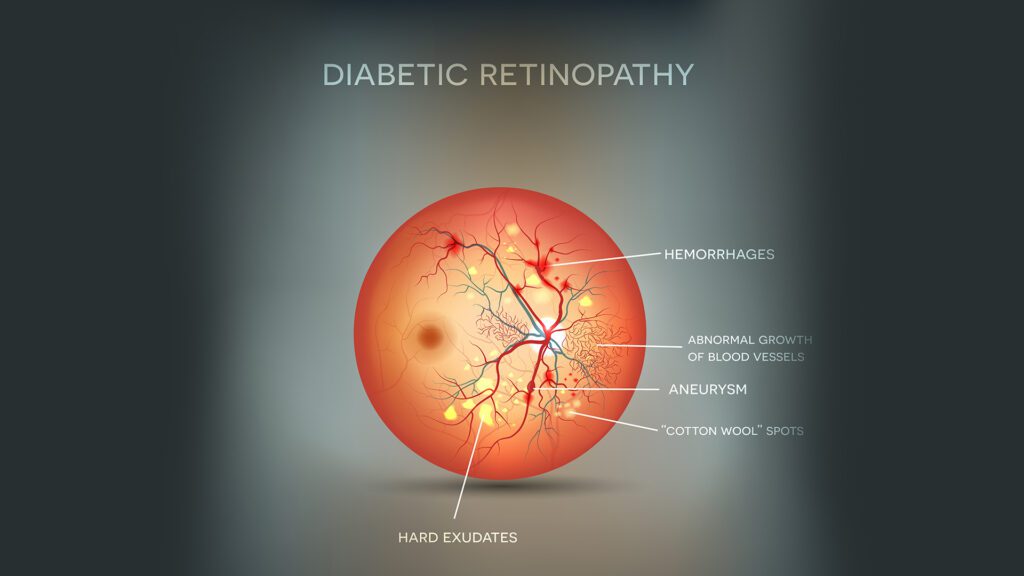
If your blood glucose (blood sugar) levels are too high for too long, it blocks off the small blood vessels that keep your retina healthy. Your eyes will try to grow new blood vessels, but they won’t develop well. The blood vessels start to weaken. They can leak blood and fluid into your retina thus causing another condition called macular edema. It can make your vision blurry.
As your condition gets worse, more blood vessels can get blocked. Scar tissue builds up due to the new blood vessels your eye has grown. This extra pressure can cause your retina to either tear or detach.
The build-up of scar tissues can also lead to eye conditions like glaucoma or cataracts (the clouding of your eye’s lens) that may result in blindness.
Risks
If you have any type of diabetes — type 1, type 2, or gestational — you may get diabetic retinopathy. Hence, the longer you have diabetes, the longer your chances are to get affected by it.
Other things that can raise your odds of having diabetic retinopathy include high blood pressure, high cholesterol and Tobacco use.
Diagnosis
Your eye doctor can usually tell if you have diabetic retinopathy during your eye test.
Pupil dilation – Your doctor will dilate your pupils to look for any changes in your eye’s blood vessels or see if any new ones have grown. They’ll also see if your retina is swollen or detached.
Fluorescein angiogram – This test can tell your doctor if you have DME or severe diabetic retinopathy. It shows if any of your blood vessels are leaking or damaged. Your doctor will give you a shot with fluorescent dye into a vein in your arm. When the dye reaches your eyes, your doctor will be able to see images of the blood vessels in your retina and spot any serious problems.
Complications
Diabetic macular edema (DME) is a serious complication of diabetic retinopathy. A healthy macula gives you sharp vision straight in front of you. This is what you need to drive, read, and see other people’s faces. If your diabetic retinopathy causes fluid buildup and swelling in your macula, you can get DME.
DME is the most common reason people with diabetic retinopathy lose their vision, and about half of people suffering from it get DME. You’re more likely to get DME at later stages of diabetic retinopathy, but it can happen at any point. At times, vision loss from DME can’t be reversed.
Prevention
Work with your doctor to maintain your blood sugar and blood pressure at good levels. This will slow down diabetic retinopathy and may even stop it from happening.
Here are more tips to prevent diabetic retinopathy:
- Make sure you see an eye doctor at least once a year for a complete eye exam.
- If you have diabetes and are pregnant, have a thorough eye exam during your first trimester.
- Follow up with your eye doctor during pregnancy. Tell your eye doctor if you develop gestational diabetes.
- Don’t smoke if you have diabetic retinopathy or diabetes.